If You Get COVID, Should You Try to Get Paxlovid? Here’s How (With or Without Health Insurance)

If you test positive for COVID and have certain risk factors that increase your chances of becoming seriously ill, you may be eligible to start a COVID antiviral treatment like Paxlovid.
Paxlovid is only available by prescription, and even if you get it prescribed, the next step is finding somewhere with enough supply to fill that prescription.
Keep reading for everything you need to know about Paxlovid and how to get it in the Bay Area, from who qualifies for Paxlovid and what “Paxlovid rebound” is, to where to find a Paxlovid prescription near you. Alternatively, use these links to jump straight to the answer you’re looking for:
How to find Paxlovid near you:
- How to get a Paxlovid prescription (no insurance)
- How to get a Paxlovid prescription (with insurance)
Key facts about Paxlovid:
- How do antiviral treatments work?
- Am I eligible for Paxlovid?
- What do we know about ‘Paxlovid rebound’?
What is Paxlovid, and should I take it?
How Paxlovid works
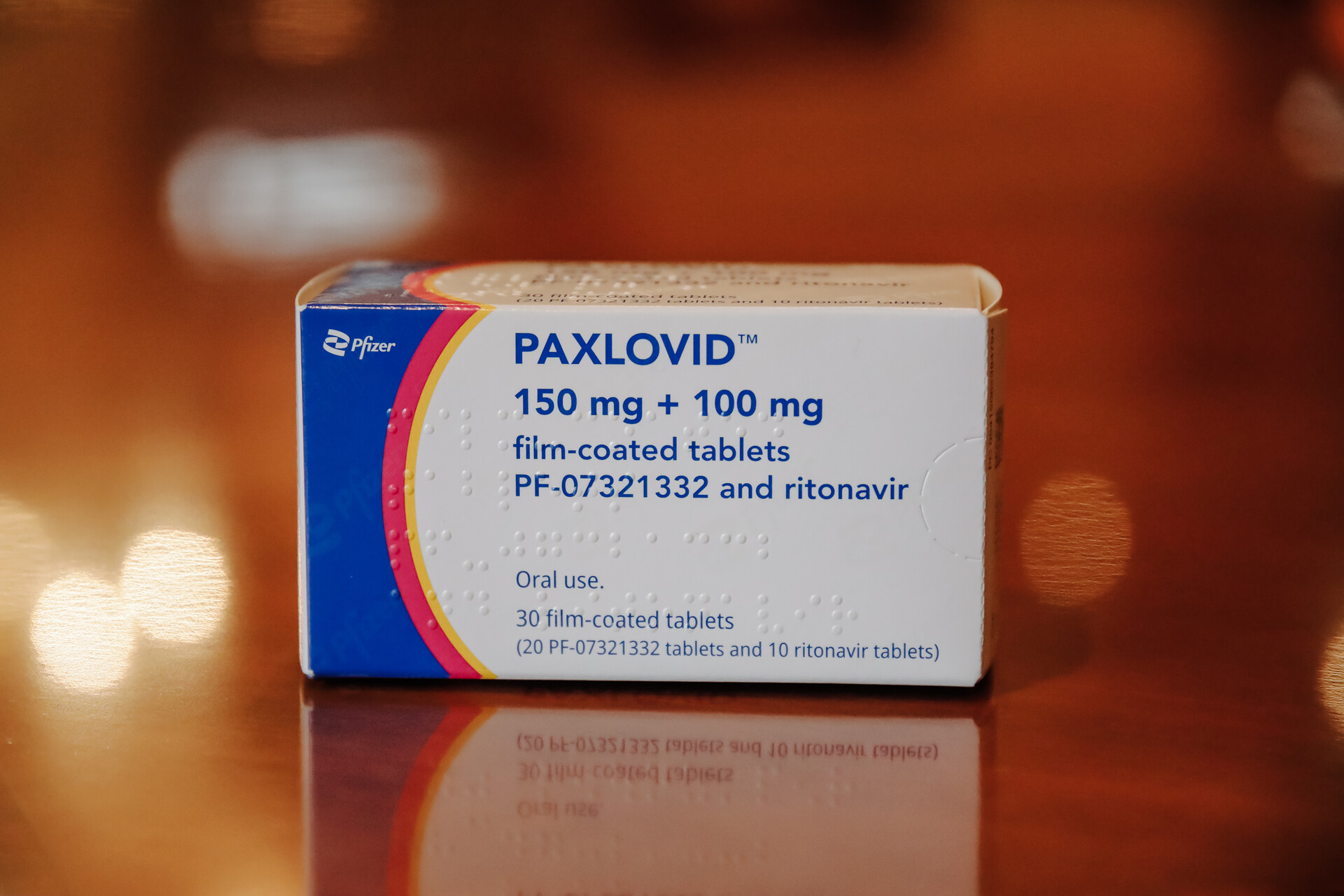
Paxlovid (pronounced “PAX-loh-vid”) is a highly effective antiviral treatment for COVID, available by prescription for people at higher risk from the disease. The treatment is over the course of five days, by taking a pill orally twice a day. Learn exactly who qualifies for Paxlovid.
Antiviral medications like Paxlovid work by stopping viruses from multiplying in the body. Studies by Paxlovid’s manufacturer Pfizer show that in unvaccinated people at serious risk of COVID complications, Paxlovid was nearly 90% effective at reducing the risk of hospitalization or death from COVID.
Paxlovid “attacks the virus in a mechanism that’s different than your immune system,” explains Dr. Bob Wachter, professor and chair of the department of medicine, University of California, San Francisco. This is particularly beneficial for immunosuppressed people whose immune systems didn’t produce a good response after getting their COVID vaccine — because “the Paxlovid should still work fine.”
While Pfizer’s Paxlovid has become a more well-known COVID antiviral drug recently, a provider may still suggest another medication for you. The other major COVID antiviral is molnupiravir, which is only available to people age 18 and over. The U.S. Food and Drug Administration’s data has shown that molnupiravir is a much less effective drug than Paxlovid, but doctors may still prescribe it in place of Paxlovid for several reasons (including the risk of Paxlovid’s interactions with other medications you’re taking).
(There are also monoclonal antibody treatments, which differ from antiviral medications. Monoclonal antibody treatments are suitable for certain people at higher risk from severe illness from COVID, and are given as a single IV injection. See the CDC’s full list of treatments available for COVID patients.)
Should I take Paxlovid if I’m eligible?
According to Wachter, starting a course of Paxlovid is the “right thing to do” if you’re high-risk and eligible for the prescription, and aren’t taking any other medications that would interfere with the treatment.
Wachter also notes that taking Paxlovid could also decrease your chances of developing long COVID. While he says the evidence isn’t yet there, Wachter’s hopeful that because Paxlovid quickly lowers the amount of virus in a person’s body, it might, in theory, “decrease the rate of long COVID.”
When should I think twice about taking Paxlovid?
For Wachter, the “judgment call” enters when your risk of hospitalization or death from COVID is low to start with — in which case you’d “be taking Paxlovid for no real benefit.” That said, it’s unlikely a provider would even prescribe you Paxlovid if they didn’t feel your personal risk factors justified it.
You may also have heard about the “Paxlovid rebound” phenomenon, which is when people taking Paxlovid start testing positive again for COVID after a week. Read more about rebound cases below.
Who qualifies for Paxlovid or other COVID antiviral treatments?
COVID antiviral treatments aren’t prescribed to every person who gets COVID.
Treatments are usually reserved for adults and children age 12 years and older who are deemed to be at higher risk for severe illness from COVID, because they have one or more risk factors or health conditions that increase their chances of becoming very sick.
According to the CDC, these include people over 65, people who are immunocompromised or have a weakened immune system, people with some types of disabilities, people with chronic liver, kidney or lung disease (including moderate to severe asthma) and people with heart conditions. See the CDC’s list of conditions that may put people at higher risk from COVID.
If you’re not sure whether you’re eligible for a COVID antiviral treatment, it’s worth getting a professional opinion on your eligibility from your own health care provider, if you have health insurance, or by visiting an Optum Serve Test to Treat location if you don’t have insurance. Don’t automatically assume you aren’t eligible — you may have risk factors you aren’t aware of that a medical professional will ask you about.
You may not also be familiar with all the conditions that put a person at higher risk for COVID. For example, the CDC’s list of possible risk factors includes mental health conditions and mood disorders like depression, and also lists being a current or former smoker.
What else do I need to know about Paxlovid and COVID antiviral treatments?
You can’t mix Paxlovid with certain other medications
“You need to make sure your doctor or the pharmacist who’s helping you understands the other drugs you’re on, because you may need to change the doses,” notes Wachter. “You may even need to stop some of them for five days.”
This is the reason it’s really important to be clear about any other medications you’re taking when you speak to a health care provider about getting Paxlovid or another COVID antiviral: Mixing them could be dangerous to your health. If you’re taking medications that would interact badly with Pfizer’s Paxlovid, a provider may prescribe you another COVID antiviral — Merck’s molnupiravir — instead.

Paxlovid and other COVID antivirals have to be taken within the first five days after you test positive
Be clear with any provider you speak with about how long ago you tested positive.
If you’ve tested positive heading into a weekend, or on the weekend itself, remember that some treatment locations may be closed at this time.
The ‘Paxlovid rebound’ is a thing
In a nutshell, the ‘Paxlovid rebound’ is when someone tests positive for COVID and takes Paxlovid, and tests negative on an antigen test for COVID after several days — but then redevelops their COVID symptoms and tests positive again on an antigen test after that. Wachter says that in these cases, the negative test comes on average on Day 7 or 8 of a COVID infection, and the positive “rebound” test and return of symptoms happens around Day 11 or 12.
How common is a Paxlovid rebound? Wachter says it’s “really a rapidly emerging story,” since only 2% of people in Paxlovid’s clinical trials experienced it but it might now seem more common among the general public because of the “amplification phenomenon of social media.” He says rebound infections “tend to be mild,” albeit lasting roughly five to seven days, and you should assume you’re infectious again if you test positive that second time.
So should the risk of a rebound infection make you think twice about taking Paxlovid? For Wachter, the benefits of the treatment are still so strong that “if I was at high risk, I definitely would take it,” he says. “But you have to have your eyes open to the possibility of rebound.”
“To me, it doesn’t change the overall benefit of practice of it, but it clearly is an area that is crying out for research,” says Wachter. “We don’t even know legitimately what percentage of people get it.”
Many people report Paxlovid has a strong metallic taste
Paxlovid is highly effective at preventing hospitalization and death from COVID, and “the side effect profile is very, very mild,” says Wachter — but “about 1 in 20 people in the clinical trials were reported to have a metallic taste in their mouth.” Or as The Atlantic puts it, “it might make your mouth taste like absolute garbage the whole time you’re taking the pills.”
Don’t be shocked if you’re one of the percentage of people who report an “altered sense of taste” from taking Paxlovid, which is temporary.
How to get Paxlovid without health insurance
What to know before you begin, if you’re uninsured
Make sure you have the following on hand:
- Proof of a positive COVID test (either a PCR result certificate or document, or your at-home COVID test itself)
- Any medications you’re currently taking, or a list of those medications (as COVID antiviral drugs can have dangerous interactions with other drugs)
Throughout the process, be clear with the provider about any symptoms you’re experiencing, and make sure they know how long ago you tested positive, since Paxlovid and other antiviral drugs must be taken within five days of a positive test.

Also, since you’re not seeing a regular provider, keep reminding any representative or health care professional you talk with, either in person or on the phone, that you don’t have health insurance and get them to confirm you won’t be asked to pay out-of-pocket costs when you’re being evaluated, when you’re being offered a prescription or when you’re filling a prescription. This may help avoid nasty surprises later down the line.
Also, be very clear with whomever you speak with that you don’t necessarily know where to fill any prescription for Paxlovid that you receive. Ask repeatedly, if necessary, where the provider recommends you fill that prescription locally — since that could end up being the hard part.
1. Find a Test to Treat site that’s run by Optum Serve
As the name “Test to Treat” implies, these locations are places where you can get tested for COVID and then potentially treated for it by being prescribed COVID antivirals on-site. Since the Test to Treat program has recently been expanded, visiting a Test to Treat site should — in theory — have gotten easier in the last several weeks.
Some Test to Treat sites also have supplies of COVID antivirals on-site, meaning you could (in theory) walk away from a Test to Treat site having been tested for COVID, evaluated for eligibility for COVID antivirals, prescribed the right treatment(s) and handed your medications.
Services at Optum Serve Test to Treat sites are free to uninsured people (this means: those Test to Treat sites run by Optum Serve, which is the federal health services business of Optum and UnitedHealth Group). So if you’re uninsured and you visit a Test to Treat location that isn’t run by Optum Serve, you could potentially find yourself asked to pay costs out of pocket.
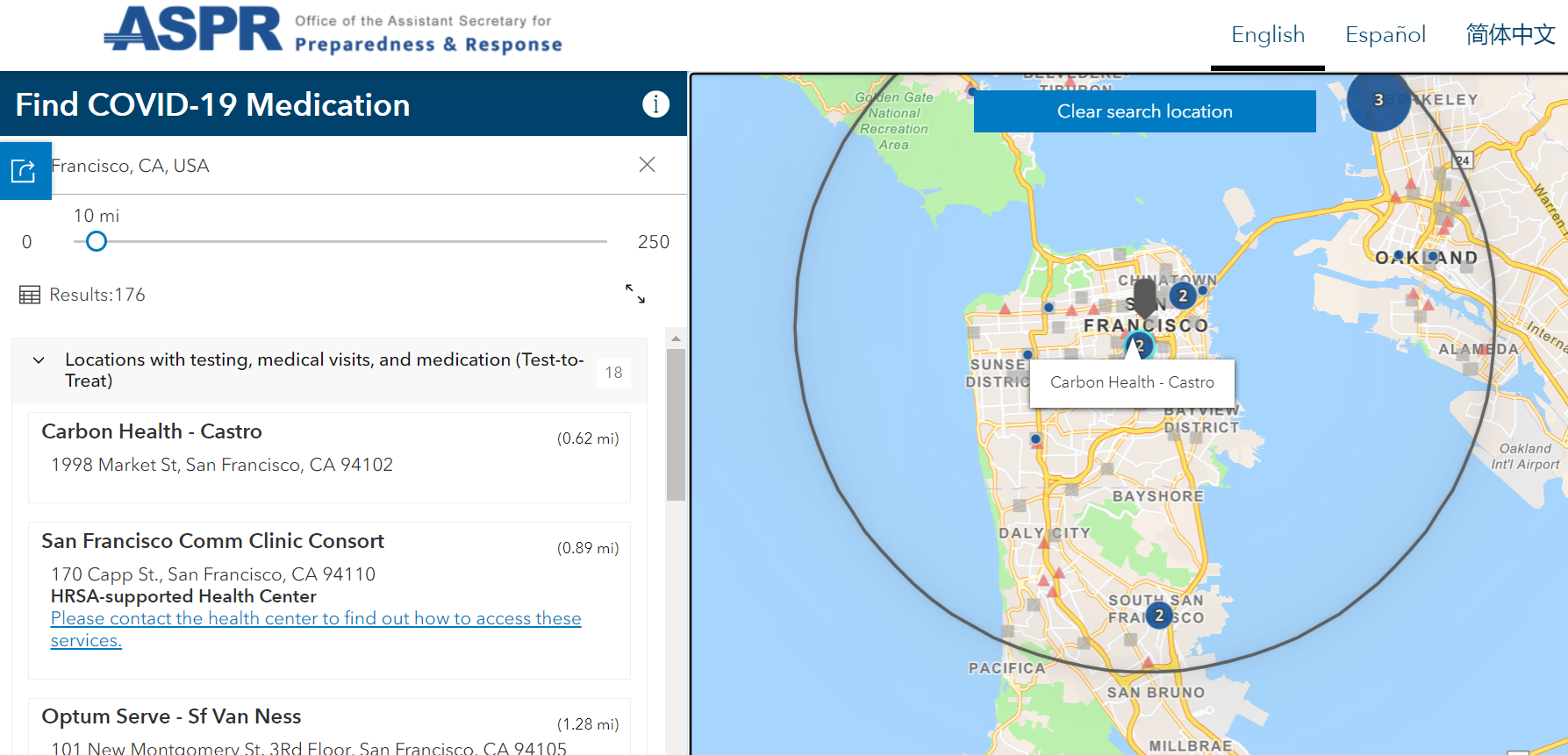
See a list of Test to Treat sites near you on the State of California’s map tool. When you input your city or ZIP code into the Test to Treat locator map, you’ll be able to see:
- Test to Treat sites themselves, i.e., locations that offer testing, medical visits and medication
- Places where you can fill an existing prescription for COVID treatment that you’ve obtained elsewhere (these locations aren’t Test to Treat sites)
If you’re uninsured and using the Test to Treat locator map to find a site, make sure you look specifically for the locations that say “Optum Serve.” You can also use Optum Serve’s own location finder tool online to see their sites on a map. The site will invite you to make an appointment for a rapid antigen COVID test and then stay on-site for your results and get medication (if eligible), all in one appointment. You can also call Optum Serve direct at (888) 634-1123. Visit the Optum Serve COVID testing and treatment site.
You can call the Test to Treat call center at (800) 232-0233 (TTY 1-888-720-7489) — assistance is available 5 a.m. to 9 p.m. PT seven days a week, in English, Spanish and more than 150 other languages. The Disability Information and Access Line (DIAL) is also available to help people with disabilities access services: (888) 677-1199, Monday-Friday, 6 a.m.-5 p.m., or email [email protected].
If the Test to Treat site you’ve visited doesn’t have supplies of the antiviral drug they’ve prescribed you, ask for staff’s assistance and advice on where you should then go to refill that prescription.
2. Visit a CVS pharmacy
How to get Paxlovid if you have health insurance
- Proof of a positive COVID test (either a PCR result certificate or document, or your at-home COVID test itself)
- Any medications you’re currently taking, or a list of those medications (as COVID antiviral drugs can have dangerous interactions with other drugs)
- Your insurance details

- Test to Treat sites themselves, i.e., locations that offer testing, medical visits and medication
- Places where you can fill an existing prescription for COVID treatment that you’ve obtained elsewhere (these locations aren’t Test to Treat sites)

This content was originally published here.


Responses