Considerations for a Local Health Insurance Option in Medicaid Non-expansion States | Milbank Memorial Fund
Policy Points
An estimated 3 million non-elderly poor adults in the 12 states that have elected not to expand Medicaid eligibility are uninsured. These uninsured adults frequently lack meaningful access to health care outside of the emergency room and other critical providers. In this brief, we propose a coverage option to fill the gap while the debate over Medicaid expansion continues in these states. Recognizing the critical role that local entities and health providers are required to play in funding care for this population, our proposal is to allow elected officials in a locality (county, city, or groups of counties) to establish an optional insurance program that takes advantage of the Affordable Care Act marketplace infrastructure and, like Medicaid expansion, is 90% funded by the federal government. This kind of program — referred to in this brief as the Local Choice Option — could provide a comprehensive insurance product that promotes appropriate access to health care and better health outcomes by repurposing funding now used only for direct care to provide health care more efficiently. This flexible program supports local customization and creates an alternative to an open-ended entitlement program in states where that is not currently politically tenable.
Background and Policy Setting
An estimated 3 million non-elderly poor adults in the 12 states that have not adopted the Affordable Care Act (ACA) Medicaid expansion are uninsured (see Table 1).1 These individuals have incomes that are above their state Medicaid eligibility threshold but below the federal poverty level (FPL), disqualifying them from both Medicaid and ACA marketplace premium subsidies and cost-sharing subsidies.2 As a result, many rural and urban communities find themselves stitching together local, state, and federal resources to pay for the care of the uninsured, and many poor and near-poor people in these states rely solely on safety-net providers for their health care needs. Many lack a source of regular health care and forgo needed preventive and primary care. Serious medical conditions are frequently diagnosed at very late stages, while low-income uninsured people cycle through emergency rooms and inpatient hospital admissions that frequently could have been avoided if they had health insurance. The result is poor health and wasteful spending.
Table 1. Non-elderly Uninsured Adults with Income under 100% FPL in 11 Non-expansion States
| State | Uninsured Individuals <100% FPL |
|---|---|
| Alabama | 141,000 |
| Florida | 564,000 |
| Georgia | 341,000 |
| Kansas | 67,000 |
| Mississippi | 120,000 |
| North Carolina | 280,000 |
| South Carolina | 140,000 |
| South Dakota | 27,000 |
| Tennessee | 177,000 |
| Texas | 1,168,000 |
| Wyoming | 11,000 |
| Total | 3,036,000 |
Source: U.S. Census Bureau. American Community Survey, 2019. Note: Wisconsin is not included here because, while it has not adopted the ACA Medicaid expansion, it uses state funds to provide BadgerCare to residents with incomes below the poverty line.
In summer 2021, two states implemented Medicaid expansion passed by ballot initiative: Oklahoma and Missouri. The remaining non-expansion states have not taken actions indicating a likely move toward it. This brief suggests a way to break the stalemate or, at a minimum, bring some important analysis and data into the conversation.
The Build Back Better (BBB) legislation that was passed by the U.S. House of Representatives and is under consideration in the U.S. Senate contains a provision that would provide subsidized health coverage through the ACA marketplaces. BBB would temporarily enable most low-income uninsured adults to qualify for premium tax credits to purchase a zero-premium benchmark plan (a silver-level qualified health plan) on ACA marketplaces beginning in 2022 and continuing through 2025. These plans would be required to cover 94% of an average person’s health care costs (actuarial value) in 2022, and in 2023–2025, this would increase to 99% of actuarial value.3
This pending federal legislation is generating an examination of the key assumptions, core components, and implementation approaches involved in local-level proposals that could offer health insurance to individuals in the coverage gap. In this brief, we outline a jointly funded (federal and local government) optional health insurance program that would operate outside of the Medicaid program and be offered alongside the marketplace. The Local Choice Option is an option that, at a minimum, provides a model for how a permanent federal–local government program can operate.
The Local Choice Option would improve health for currently uninsured people without impeding a state’s ability to choose Medicaid expansion later. Moreover, it can be designed with an awareness of the implications of coverage changes for hospitals’ disproportionate share hospital (DSH) funding, provider taxes, and other revenue streams.
Essential Features of a Local Choice Option Program
The way localities have effectively been required to provide care to uninsured people is inefficient and costly. Many counties support hospitals and clinics using a patchwork of complex tax authorities and financial arrangements between state governments, federal agencies, and health care delivery systems. These arrangements have developed in ad hoc ways that do not serve providers, local governments, patients, or taxpayers well. All these groups would benefit if localities had access to funds for the purchase of an insurance product for uninsured, non-elderly, documented individuals with incomes under 100% of the FPL.
The Local Choice Option program would involve a modest investment, with 90% of funding covered by the federal government, that could bring the benefits of comprehensive health insurance to the residents in the non-expansion states who live in poverty but do not qualify for these states’ traditional Medicaid programs.
The Concept: Localities Authorize a Coverage Program for Low-Income Uninsured People
A Local Choice Option program would allow a locality (county, city, or groups of counties) to secure and obtain federal support for insurance coverage of low-income uninsured adults in non-expansion states. This coverage, which could be provided through an insurance platform such as the ACA marketplace, would have the following key characteristics.
Program Characteristics
Local Choice. The decision to authorize and thereby opt into the program is entirely left to the locality. Both rural and metropolitan entities are eligible. Rural providers face substantial access and financing challenges, and Medicare’s Critical Access Hospital revenue meets only a portion of this need. Creating a health insurance coverage path for rural localities could help address residents’ primary and preventive health needs, respond to the opioid crisis, and assist with telehealth access and transportation to providers’ offices and clinics.
The local entity would apply for the participation and provide proper assurances that lay out terms and conditions of its relationship with the federal government. Funds would flow directly from the federal government to the local government entity. The Health Resources and Services Administration (HRSA), which has a long history of funding localities for a wide range of health-related needs, or a similar federal agency, could be the federal government’s administrative agency for the program.
Medicaid-like Coverage without Medicaid Entitlement. The Local Choice Option would not be part of Medicaid, nor would it trigger entitlement to coverage. Rather, it would provide an interim, non-entitlement option just in the non-expansion states. Although a local initiative would construct a “Medicaid look-alike” benefit and actuarial value comparable to Medicaid rates for the coverage, it would have program flexibility within certain parameters. For example, if the county committed to cover at least half the eligible residents, a county with 20,000 eligible uninsured residents might calculate that it can serve 10,000 eligible individuals in fiscal year (FY) 2023. After its experience in the first year, the county may then determine that it is able to enroll 12,000 people in FY 2024. With such information and forecasted per member per month (PMPM) costs, counties could construct a fixed budget for the program and reauthorize it as long as it continues to benefit members effectively. The Local Choice Option coverage could be integrated with a state program if statewide Medicaid expansion is initiated later.
Localities would likely want some assurance that the federal contribution would not be quickly pulled or amount to a “one-and-done” arrangement. To address both this concern and honor the concept of avoiding an open-ended entitlement, counties might seek a multiyear commitment from the federal government, such as a minimum of five years of federal funding. This assumes that the new county program is successfully implemented in the first year.
Federal Funds and Local Match Support a Medicaid Look-alike. The Local Choice Option program would mirror state Medicaid coverage with benefits identical to the state’s Medicaid program. The federal entity would essentially lay out the rules for the program and the participating qualified health plans (QHPs), many of which already serve Medicaid members. The participating local entity would fund the 10% non-federal share that the state would have paid under Medicaid expansion. Nationally, the federal match would fund an approximately $12.6 billion program annually ($11.34 billion federal and $1.26 billion local at $350 PMPM). These cost figures assume a 50% participation rate among counties. Local Choice Option enrollment may increase gradually and could be lower than 50% initially. Adjusting the funding to be 100% federal would increase the federal outlay by less than $1 billion annually.
Redeploying Funding to Support Comprehensive Health Coverage. An essential feature of the Local Choice Option program is the reallocation of a portion of local funding that currently directly funds safety-net providers to support affordable, comprehensive health coverage. In addition to providing patients with a more meaningful source of assistance, the new coverage will provide Medicaid-level payments to providers already serving those patients, often without being reimbursed. While the Local Choice Option payments will be below commercial and Medicare rates, for hospitals and community health centers providing nearly free care, they are still preferable to receiving no payment. This also helps reduce hospitals’ attempts to recover patient debt and helps individuals avoid medical bankruptcies.
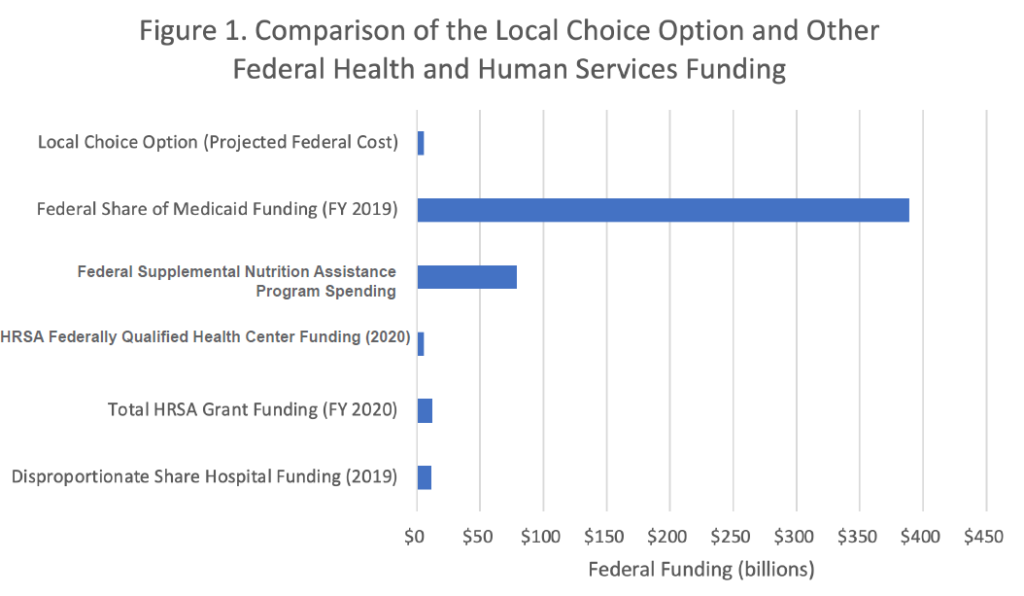
Creating a More Reliable, Better Coordinated Funding Infrastructure for Localities and States. The overlap and inefficiencies built into the current maze of funding hinders access to affordable health care for low-income people. The Local Choice Option can streamline and improve access to care by offering better-designed coverage to enrollees. Redeploying resources for affordable health insurance also creates opportunities for locally designed financial accountability and increased efficiencies. As shown in Figure 1, Local Choice Option funding is relatively small compared with current federal funding streams supporting health care and related services for low-income populations.
Table 2 identifies existing HRSA grant funding to five large counties in non-expansion states. The amount of direct funding from the federal government to states is already substantial and reflects just one dimension of funding that could be coordinated with a potential insurance product.
Sources: Health Management Associates estimates, HRSA, MACPAC (Medicaid and CHIP Payment and Access Commission), U.S. Department of Agriculture, Urban Institute estimates based on data from the Centers for Medicare and Medicaid Services (Form 64), as of August 2020.
Table 2. HRSA Funding by County
| County | HRSA Funding 2021 |
|---|---|
| Dallas County, Texas | $66 million |
| Fulton County, Georgia (Atlanta) | $181 million |
| Harris County, Texas (Houston) | $144 million |
| Jefferson County, Alabama (Birmingham) | $35 million |
| Miami-Dade County, Florida | $180 million |
| Total | $606 million |
Source: HRSA. Awarded Grants by State and County. https://data.hrsa.gov/data/reports/datagrid?gridName=FinancialAssistance. Accessed January 20, 2022.
Operational Considerations
Establishing a new program always takes significant effort, but existing infrastructure and authorization pathways provide a roadmap for the establishment of Local Choice Option programs.
Leveraging Existing Eligibility and Enrollment Infrastructure. Currently, in the states with the most potential for Local Choice Option opportunities (see Table 1), the federally facilitated health insurance marketplace — as opposed to a state-run marketplace — provides commercial QHP and premium subsidy/cost sharing reduction eligibility and enrollment functions.
Although adding a non-Medicaid, non-marketplace insurance offering to the existing marketplace offerings will require significant technical and system adjustments, the Centers for Medicare and Medicaid Services (CMS) could build functionality for a Local Choice Option for eligible populations. The Local Choice Option product(s) would have to complement, not conflict with, commercial products and Medicaid benefits available locally. Additionally, the capabilities and vendor contracts that CMS has in place to facilitate enrollment into QHPs, make advanced premium tax credit payments to health plans, and regulate benefit and payment parameters could be leveraged to provide centralized, core business operations for the Local Choice Option — much in the way that CMS currently supports states with a federally facilitated marketplace.
While the program should be crafted so that it would be minimally invasive for the local governments (e.g., authorization and funding would be the two key responsibilities), the federal governing entity would need to support the Local Choice Option by providing dedicated resources for technical assistance (i.e., not an “add-on” to existing jobs) for local jurisdictions considering a Local Choice Option program. In particular, funding efforts could focus on assisting jurisdictions with decision-making, budgeting, and evaluations of Local Choice Option implementation. This assistance, along with the operational and administrative function support provided by the federal government, would reduce the technical and financial burden for local governments and encourage widespread implementation of Local Choice Option programs.
HRSA could serve as the lead federal agency for Local Choice Option administration, financing, and technical assistance. Although some functions required for implementing the Local Choice Option, such as benefit development and financing, would be new for the agency, HRSA already provides substantial funding to localities through programs such as the Ryan White HIV/AIDS Program, Maternal and Child Health grants, and support for rural health. Federally qualified health centers that receive such funding could serve as enrollment hubs. HRSA would have to coordinate with CMS for establishment of benefit standards. One important qualification would involve the need to ensure that the new diagnosis code for long COVID receives adequate HRSA funding; we estimate that the current HRSA funding that supports care for uninsured people would be sufficient to cover primary care and behavioral health as well as COVID and long-COVID care.
Benefit of the Local Choice Option
Counties have experience with populations and federal funding. It is very common for US counties and other local governments to raise revenues and fund health care for low-income populations. Many counties have extensive experience working with local health systems and braiding federal and local resources. Counties receive a variety of federal government funding streams that support their provision of health care services for low-income and vulnerable populations.
For major counties in the current patchwork financing system, the locally controlled contribution amounts are substantial and could constitute the required 10% local contribution. Three examples of local contributions are the following:
Any change in the funding streams for large and locally important health care providers will generate concern and resistance. The Local Choice Option would have to be designed with an awareness of the implications of coverage changes for DSH funding, provider taxes, and other revenue streams that could be affected by reducing the number of uninsured people. A few related issues regarding our examples are as follows:
Because providers will be reimbursed for services to individuals newly covered by a Local Choice Option insurance product, this will impact eligibility for DSH, supplemental payments, and other revenue streams. The illustrations use conservative estimates to account for potential cuts. The revenue payoff of a Local Choice Option will substantially increase the total available funds, given that a 90% match is greater than the traditional Medicaid FMAP and a good portion of the 3 million uninsured people in non-expansion states would be categorically eligible for the Local Choice Option.
An insurance-based product aligns patient and provider incentives. Significant research shows that individuals without insurance coverage are more likely to lack a regular source of care, put off seeking care, and have poorer health outcomes than those with coverage.4 While individuals getting care from community health centers have reduced out-of-pocket costs, they frequently face co-payments on a sliding scale, which can be a barrier to seeking primary or preventive care.
Offering low-income individuals an established insurance product is a more systematic approach to increasing the accessibility and provision of health care for uninsured populations relative to the current byzantine process. Further, it should help rural localities address such serious problems as the opioid crisis, COVID-19, and the need for access to timely health services, including telehealth and non-emergency transportation.
In addition, this approach holds the potential for obtaining some bipartisan support. Reduced numbers of uninsured people may result in lower commercial premiums since any provider subsidies for uncompensated care incorporated into those rates would be less necessary.
Some of those opposed to Medicaid expansion may see the Local Choice Option as preferable to the ACA Medicaid expansion. Some proponents of the expansion may see this option as an opportunity to allow coverage to begin in states that have not expanded Medicaid, which, if successful, could point the way toward future statewide coverage expansion. As Local Choice Option programs show results, they can serve as models that could be scaled up later.
The Local Choice Option would increase funding reliability for care paid for at the local level. The federal administration’s reconsideration of the previously approved Texas Medicaid waiver changes the dynamics of health care funding for low-income, uninsured populations and puts the federal, state, and local governments in a position to think through alternative financing ideas. The Texas waiver is a good illustration of the complexities and inefficiencies of the current system, as it would have reimbursed approximately $11.4 billion a year to Texas hospitals providing uncompensated care through 2030.
Our current system reimburses hospitals for acute care, but we spend much less to organize and finance primary and preventive care for uninsured people that would help them avoid inpatient care. The Local Choice Option presents an opportunity to reduce such inpatient admissions and readmissions. Front-end coverage helps reduce flare-ups and complications from chronic illnesses. Of particular interest are funding programs that offer comprehensive coverage rather than fund care on an ad hoc basis. The Local Choice Option could greatly stabilize the funding stream and allow local authorities to opt in if they choose to do so.
Given that the Local Choice Option population would be a subset of those who could be affected by a statewide Medicaid expansion, it is possible that the program would not require additional federal financial offsets from a Congressional Budget Office (CBO) scoring point of view. CBO could take the position that federal funding for the Local Choice Option is already in its baseline forecasts.
Program Limitations
While beneficial for the individuals in a locality that takes up the Local Choice Option approach, the program would provide new coverage only to a subset of those in need. This subset would have to be identified and prioritized by the locality. The coverage would not be guaranteed and could be discontinued by the local entity at any time. Even with the best of intentions of minimizing local efforts and aligning with existing federal marketplace programs and benefits, the Local Choice Option would create new administrative processes for providers, patients, insurers, and governments.
Expansion advocates may also be concerned that local programs could take the steam out of efforts to get non-expansion states to adopt the Medicaid expansion. We maintain that hundreds of thousands, if not millions, of uninsured people do not have time to wait for these decisions to be worked out — they need an alternative to break the stalemate.
Avoiding the entitlement nature of Medicaid, avoiding any claim on state funding, and enhancing local choice are all features that should provide some financial predictability and appeal to those who opposed Medicaid expansion. Getting Medicaid-equivalent coverage to a substantial portion of those now caught in the coverage gap should appeal to ACA supporters, as well as to local providers and Medicaid managed care organizations. Waiving the entitlement feature for these important pilot projects, however, does not in any way interfere with the long-standing entitlement nature of Medicaid.
Summary and Conclusions
1 U.S. Census Bureau. American Community Survey. 2019.
2 Garfield R, Orgera K, Damico A. The coverage gap: uninsured poor adults in states that do not expand Medicaid. Kaiser Family Foundation. https://www.kff.org/medicaid/issue-brief/the-coverage-gap-uninsured-poor-adults-in-states-that-do-not-expand-medicaid/. Published January 21, 2021. Accessed January 10, 2022.
3 Park E, Corlette S, Dwyer A, Clark M. Build Back Better Act: health coverage provisions explained. Georgetown University Health Policy Institute, Center for Children and Families. https://ccf.georgetown.edu/wp-content/uploads/2021/11/Build-Back-Better-FINAL-Nov19.pdf. Published November 2021. Accessed January 10, 2022.
4 Tolbert J, Orgera K, Damico A. Key facts about the uninsured population. Kaiser Family Foundation. https://www.kff.org/uninsured/issue-brief/key-facts-about-the-uninsured-population. Published November 6, 2020. Accessed January 21, 2021.
Citation:
Meyer J, Powers M, Leibowitz N. Considerations for a Local Health Insurance Option in Medicaid Non-expansion States. The Milbank Memorial Fund. Published February 3, 2022.
This content was originally published here.


Responses